45/F with itchy skin lesions over back, hands, neck and face
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
Chief complaints:
Patient c/o itchy skin lesions over back, hands, neck, face since 3 months.
C/o fever since 2 months (1episode every day)
C/o oral ulcers since 1 month
C/o joint pain since 15 days
HOPI:
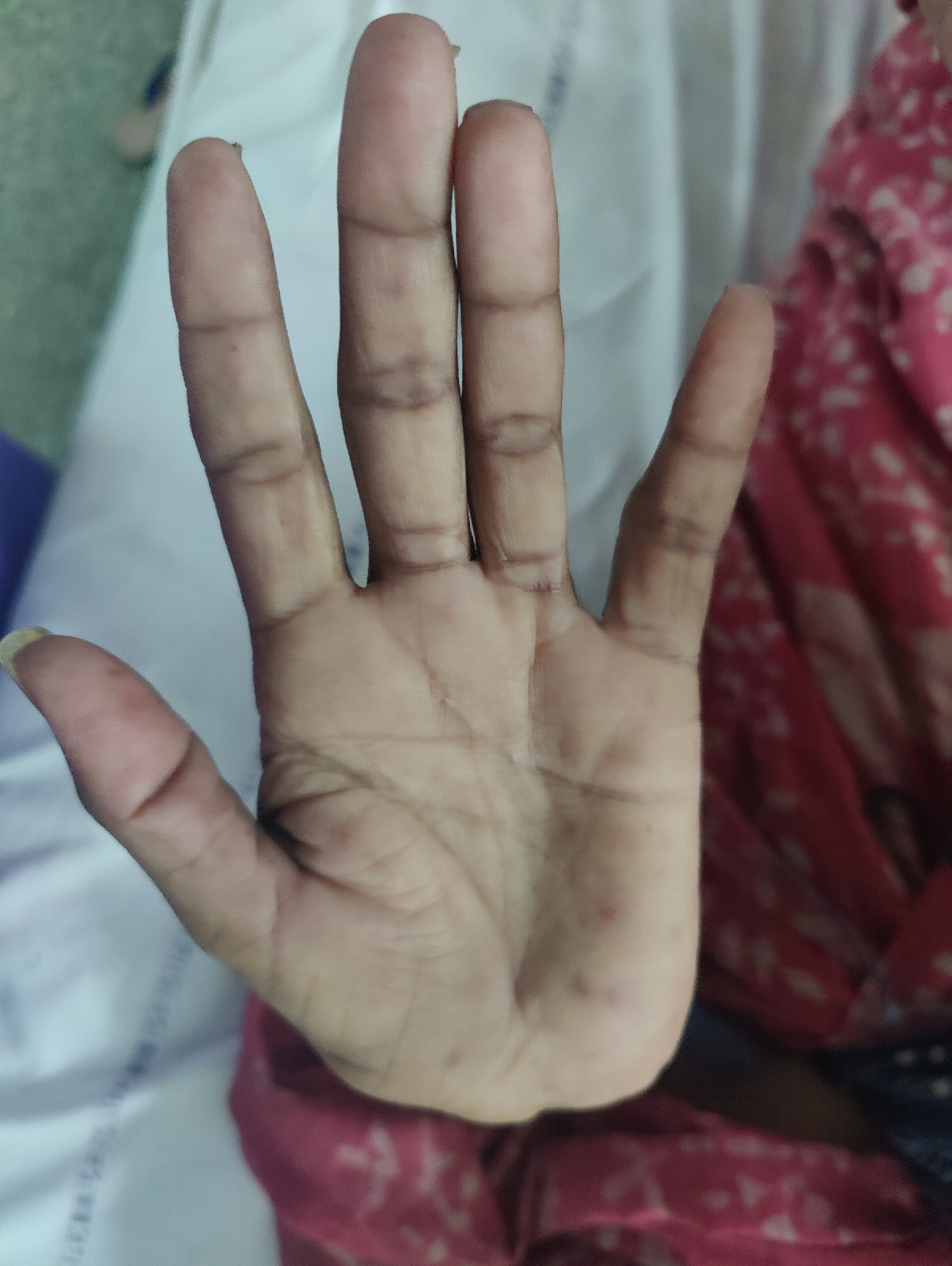
Patient was apparently normal 3 months back, when her complaints started as itchy skin lesions over back which progressed to hands.
C/O high grade, continuous fever, 1 episode per day, relieved on taking medication.
H/o painful oral ulcers since 1 month, associated with difficulty in swallowing and burning sensation.
C/o joint pains since 15 days associated with swelling
No h/o morning stiffness.
H/o photosensitivity present.
H/o usage of
- TAB. OMNACORTIL 30MG
- TAB AUGMENTIN 625MG
- BETAMETHASONE LOTION
- CANDID MOUTH PAINT
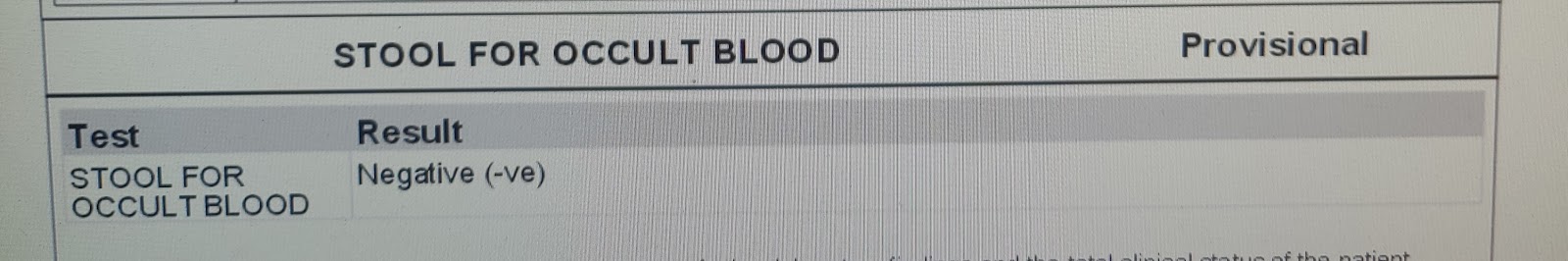
No occult blood present in stools.
No h/o new drug intake prior to symptoms
No h/o dry eyes, mouth, raynauds phenomenon
No h/o chest pain, dysnea, palpitations
Past history:
K/c/o elephatiasis of right leg since 30 years
N/K/C/O DM2, HTN, CAD, ASTHMA, TB, EPILEPSY, CVD, CAD, THYROID DISORDER
General Examination :
Patient is examined in a well lit room after taking informed consent.
Patient is conscious, coherent and cooperative.
She is moderately built and moderately nourished.
Pallor: Present
Icterus: absent
Cyanosis: absent
Clubbing: absent
Generalized Lymphadenopathy: Absent
Edema: Absent
Vitals:
Temp: 97F
BP: 120/80mmhg
PR: 84 bpm
RR: 16 cpm
GRBS: 98
SYSTEMIC EXAMINATION :
CVS : S1 S2 heard. No murmurs
RS : Bilateral air entry present
CNS : no focal neurological deficit
P/A : soft non tender
Skin:
O/E:
Multiple oral ulcers noted over bilateral buccal mucosa, hard palate
Multiple polysized hyperpigmentated plaques with crusting noted over face, neck, hands, back, abdomen.
Diffuse loss of hair over scalp
Non pitting edema of right lower limb
Multiple polysized hyperpigmentated macules noted over bilateral cheeks, forehead.
ECG:
29/05/23
30/05/23:
02/06/23
X-ray spine:
Impression:
Mild degenerative changes notes in the cervical spine.
Ophthal referral:
On fundus examination, no changes of hypertensive retinopathy, noted in both eyes. .
Gastroenterology Referral:
Esophageal candidiasis
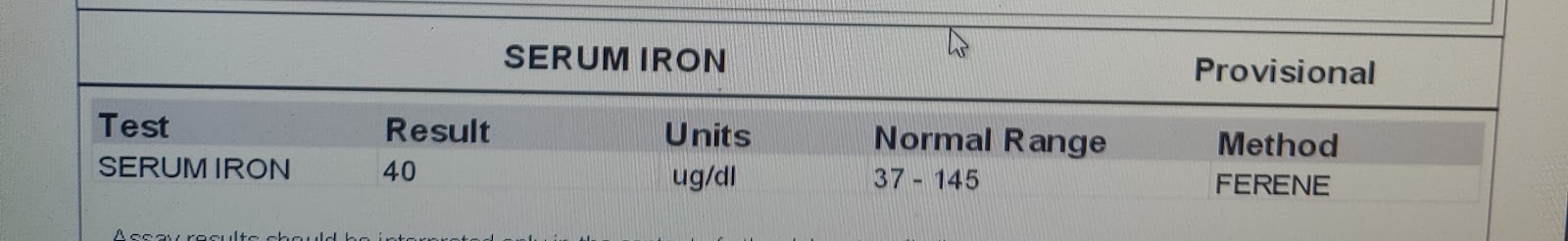
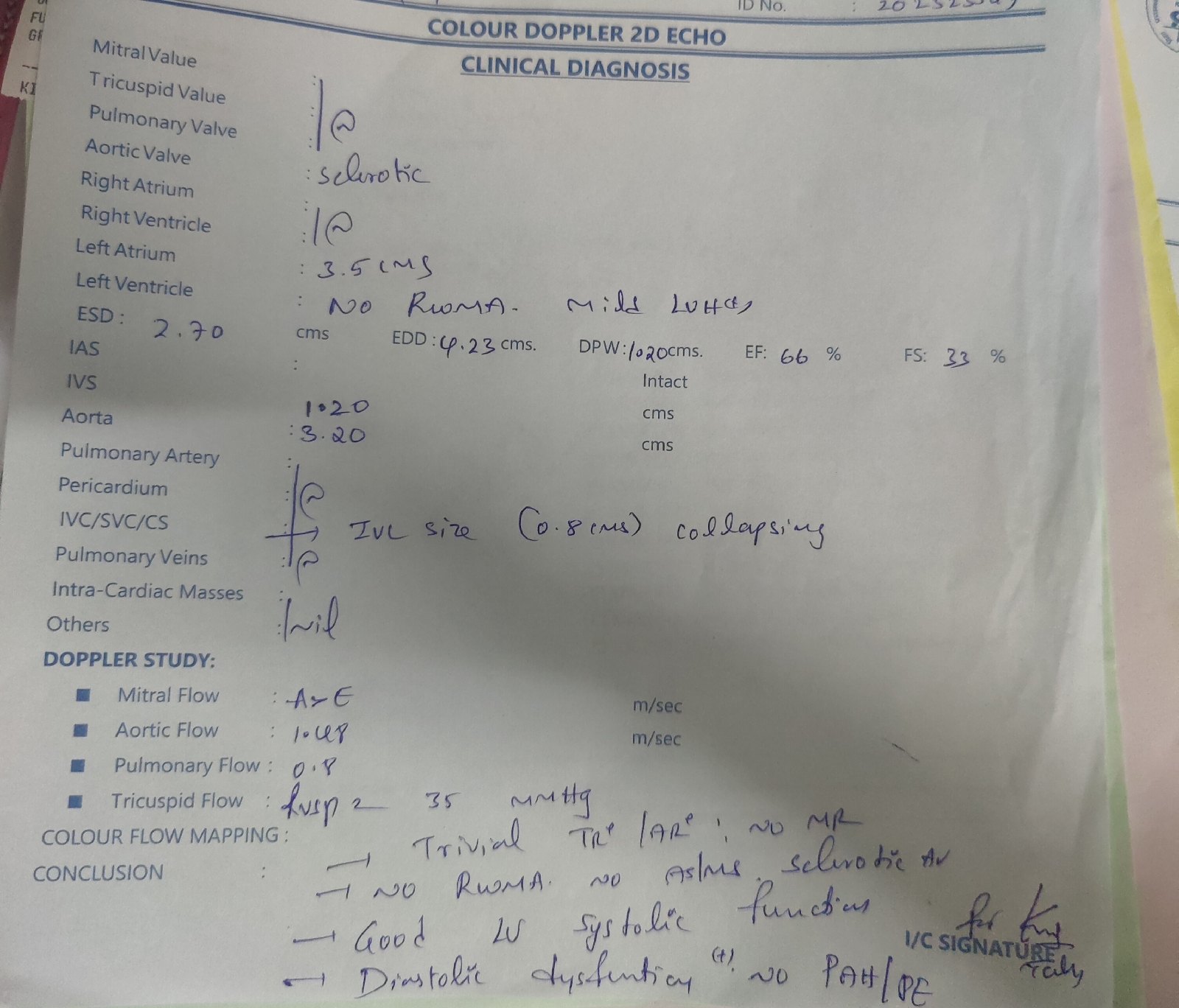
2D echo:
Treatment:
1. TESS PASTE L/A TID (20MIN BEFORE FOOD)
2. TAB. TECZINE 10MG OD
3. SUNCROS AQUAGEL L/A SPF 50 TID
4. TAB. ZINCOVIT OD
5. FUDIC CREAM L/A BD
6. TAB. PREDNISOLONE 20MG OD
7. TAB. PAN 40MG OD (BBF)
8. TAB. TELMA 40MG PO/OD AT 8AM































Comments
Post a Comment